Crystalluria indicates that the urine is supersaturated with the compounds that comprise the crystals, e.g. ammonium, magnesium and phosphate for struvite. Crystals can be seen in the urine of clinically healthy animals or in animals with no evidence of urinary disease (such as obstruction and/or urolithiasis). However, some crystals can be pathologically relevant in certain circumstances (see example of ammonium biurate below). Note that crystals may not form in all urine supersaturated with these compounds. A number of in vivo and in vitro factors influence the types and numbers of urinary crystals in a given sample as indicated in the table below.
|
|
Crystals are identified by their characteristic shape and the pH of the urine in which they occur (see crystal quick guide). It can be difficult to differentiate between certain types of crystals, e.g. xanthine and ammonium biurate, and the dissolution characteristics of the crystals in strong acids or alkali can be used to facilitate crystal identification (see below). Ultimately, however, optical crystallography or high pressure liquid chromatography are the optimal method for identification.
Crystals are subjectively quantified in urine as few, moderate and many. For crystals that are large, e.g. calcium carbonate and struvite, this assessment is made from low power (10x objective). For smaller crystals (e.g. amorphous, calcium oxalate dihydrate), the high power (40x objective) is used. Additional information on some specific crystals seen in urine are given below.
| Common crystals | Uncommon crystals |
| Struvite | Calcium oxalate monohydrate (picket fence form) |
| Bilirubin | Ammonium biurate |
| Calcium carbonate | Cystine |
| Amorphous | Drug-associated |
| Calcium oxalate dihydrate or monohydrate (oval or dumb-bell forms) | Other |
Struvite

Struvite crystals (magnesium ammonium phosphate, triple phosphate) usually appear as colorless, three-dimensional, prism-like crystals (“coffin lids”). Occasionally, they instead resemble (vaguely) an old-fashioned double-edged razor blade (lower frame). They are usually large and can be readily observed at low magnification (however, confirmation of crystal identity should always be performed under high magnification). Struvite crystals are the most common type in urine from dogs and cats. They are often seen in urine from clinically normal individuals. Though they can be found in urine of any pH, their formation is favored in neutral to alkaline urine. Urinary tract infection with urease-positive bacteria can promote struvite crystalluria (and urolithiasis) by raising urine pH and increasing free ammonia. They are birefringent with polarized light.
Bilirubin
Bilirubin crystals form from conjugated bilirubin (water soluble) and are needle-like to granular crystals that are yellow in color. They tend to precipitate onto other formed elements in the urine. In the top picture, fine needle-like crystals have formed on an underlying cell. This is the most common appearance of bilirubin crystals. In the lower two pictures, cylindrical bilirubin crystals have formed in association with droplets of fat, resulting in a “flashlight” appearance. This form is less commonly seen. They are usually small crystals that are usually only observed at high magnification (unless there are large aggregates of crystals). Bilirubin crystals are seen most commonly in canine urine, especially in highly concentrated specimens. They are less common in urine of other species. In dogs, they often are of no clinical significance (healthy dogs can have low, but detectable, bilirubin levels in urine). Bilirubin crystals (or a positive chemical reaction on the urine dipstick) in feline, equine, bovine, or camelid urine is an abnormal finding and the animal should be investigated for an underlying cholestatic process.
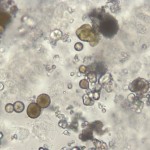
Calcium carbonate
Calcium carbonate crystals are variably sized crystals that frequently appear as large spheroids with radial striations. They can also be seen as smaller crystals with round to ovoid shapes. they are colorless to yellow-brown and can impart a brownish tinge to the urine, when they occur in high numbers. They are usually large crystals and can be readily observed at low magnification (however, confirmation of crystal identity should always be performed under high magnification and smaller variants of calcium carbonate may be missed if only low magnification is used). These crystals are common in the urine of normal horses, rabbits, guinea pigs and goats. They have not been observed in canine or feline urine.
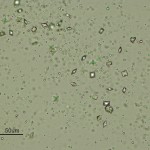
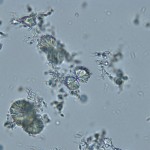
“Amorphous” crystals
“Amorphous” crystals appear as aggregates of finely granular material without any defining shape at the light microscopic level. They can be comprised of urates, phosphates or xanthine. They are usually small crystals that are usually only observed at high magnification (unless there are large amounts of them), i.e. they mimic bacteria.
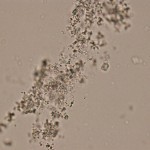
Amorphous urates (Na, K, Mg, or Ca salts) tend to form in acidic urine and may have a yellow or yellow-brown color (on sedimentation, the urine can look pink if there are sufficient cyrstals). Amorphous phosphates are similar in general appearance, but tend to form in neutral or alkaline urine and lack color. Xanthine crystals are usually in the form of “amorphous” crystals, however some can resemble ammonium biurate (Hooijberg et al, www.escvp.org case). These crystals occur in Dalmations on allopurinol therapy for urate urolithiasis. Generally, no specific clinical interpretation can be made based on the finding of amorphous crystals. Small amorphous crystals can be confused with bacterial cocci in some cases, but can be distinguished by gram-staining. Degenerating cells can also resemble “amorphous” crystals.
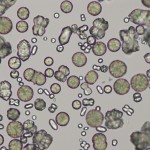
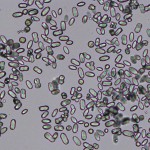
Calcium oxalate dihydrate
Calcium oxalate dihydrate crystals typically are colorless squares whose corners are connected by intersecting lines (resembling an envelope). They can occur in urine of any pH. The crystals vary in size from quite large (can be observed under low magnification) to very small (require big magnification to visualize). In some cases, large numbers of tiny oxalates may appear as amorphous unless examined at high magnification. These crystals are often seen in normal urine from domestic animals and can also be an artifact of storage (they can develop in stored urine), emphasizing the need to perform a urinalysis on fresh urine samples. They are birefringent with polarized light.
Urolithiasis due to calcium oxalate has been reported in both dogs and cats. In some cases, they occur secondary to abnormal calcium (increased) excretion due to disorders of calcium metabolism (e.g. hyperparathyroidism). Miniature Schnauzers are predisposed to calcium oxalate urolithiasis, despite no abnormalities in urinary calcium excretion. Calcium oxalate dihydrate crystals can also be seen in cases of ethylene glycol intoxication, although the picket-shaped form of calcium oxalate monohydrate are more specific for this toxicosis (see below) and not seen in the urine from healthy animals. If seen in large numbers in the urine of a dog or cat with acute renal failure and other appropriate clinical signs, consideration should be given to this diagnosis.
Calcium oxalate monohydrate
Calcium oxalate monohydrate crystals vary in size and may have a spindle, oval, or dumb-bell shape (for examples, see the two unlabeled crystals in the lower left corner of the image below right). These forms of calcium oxalate monohydrate indicate supersaturation of the urine with calcium and oxalate and, along with calcium oxalate dihydrate crystals (“square envelopes”), can be seen in the urine of animals that have no urologic problems or those suffering from oxalate urolithiasis, hypercalciuric or hyperoxaluric disorders, or rarely ethylene glycol toxicosis. They are infrequent in the urine of normal dogs and cats but can be seen in the urine from healthy horses. These can be seen at low magnification, however low numbers may only be identified at high magnification (and crystal identity should be verified under high magnification, particularly due to the pathologic relevance of the “picket fence” form of these crystals).

A particular form of calcium oxalate monohydrate are flat, elongated, six-sided crystals (“picket fences”) which are the larger crystals in the image above (which represents urine from a dog with ethylene glycol toxicosis). The arrow in the photo indicates a “daughter” crystal forming on the face of a larger underlying crystal. These “picket fence” forms of calcium oxalate monohydrate are frequently associated with ethylene glycol intoxication in dogs and cats, but are not always observed in the urine of affected animals (i.e. not 100% sensitive). They can also be seen in the urine of animals with hypercalciuria from other causes, e.g. paraneoplastic hypercalcemia with lymphoma. Another rare form of calcium oxalate monohydrate are the “hempseed” variant or “orzo” (as in the pasta shape). The left image above is from the urine of a dog with many of these crystals. The dog did not have ethylene glycol poisoning and the crystals are assumed to be secondary to supersaturation of the urine with calcium and oxalates, which precipitated in the acidic urine.
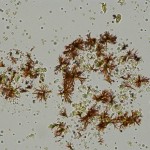
Ammonium biurate
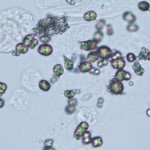
Ammonium urate (or biurate) crystals generally appear as brown or yellow-brown spherical bodies with irregular protrusions (“thorn-apples”). In some urine samples, they do not have irregular protrusions but have smooth borders and can resemble calcium carbonate (although these do not occur in the urine from dogs and cats). These crystals can be observed under low magnification, particularly when seen in large number, however low numbers may only be seen at higher magnification. Due to their potential pathologic relevance, crystal identification should be verified by examination at high magnification. Though possible in urine of any pH, their formation is favored in neutral to acidic urine. They are frequently seen with amorphous urates. These crystals are fairly common in dogs and cats with congenital or acquired portal vascular anomalies, with or without concomitant ammonium urate uroliths. They have been seen in animals on chemotherapy with increased uric acid production . They can be seen in urine from normal Dalmatians, English Bulldogs and Black Russian terriers, due to a defect in a putative urate transporter (SLC2A9 gene; mutation of cysteine to phenylalanine at amino acid 181) (Karmi et al 2010), with Dalmations and English bulldogs being predisposed to urate urolithiasis (Barges et al 1994, Bende and Németh 2004, Houston et al 2004). They are rarely, if ever, seen in urine from normal cats or dogs of other breeds and have not been reported in large animals.
Cystine

Cystine crystals are flat colorless plates and have a characteristic hexagonal shape with equal or unequal sides. They often aggregate in layers. Their formation is favored in acidic urine. These crystals vary in size from small to medium and should be visible to some extent under low magnification (as always, identification should be verified under high magnification). Cystine crystalluria or urolithiasis is an indication of cystinuria, which is an inborn error of metabolism involving defective renal tubular reabsorption of certain amino acids including cystine. Sex-linked inheritance is suspected since male dogs are almost exclusively affected. Many breeds, as well as mongrels, have been reported affected . Renal function otherwise appears to be normal and, aside from a tendency to form uroliths, the defect is without serious consequence (for more on cystine uroliths, please refer to our diagnostic challenge November 2018). They are not birefringent with polarized l ight.
Drug-associated crystals
Many drugs excreted in the urine have the potential to form crystals. Hence, a review of the patients drug history is prudent when faced with unidentified urine crystals. These crystals vary in size and larger variants or many crystals are observed under low magnification. Most common among these are the sulfa drugs. Both panels on the right are from patients receiving trimethoprim-sulfadiazine. The differing appearance may relate to variation in drug concentration, urine pH, and other factors. See the image to the right for crystals in urine from a dog that were presumed to be drug-associated. Other tests can be used to support the presence of drug crystals. For example, the lignin test can be used to identify sulfonamide crystals. In this test, a yellow color forms on a drop of urine on paper when a drop of 10% hydrochloric acid is added (Miller et al 2011). The acid reacts with aminophenyl groups in sulfonamides, but other chemicals or drugs containing such groups will cause a similar reaction, including the vitamin B (Moerke 1944).
Other examples include radiopaque contrast agents (Hypaque, Renografin) and ampicillin which may precipitate in acid urine as fine needle-like crystals (not shown).
Other crystals
We frequently see several different types of crystals that are of uncertain origin (see urine sediment atlas for examples). Whenever an “unknown” crystal is encountered, we usually perform solubility studies (chemical, i.e. hydrochloric acid, glacial acetic acid and sodium hydroxide, or heat) to help identify the crystals. Some crystals, such as uric acid, calcium phosphate and sulfa drug-related crystals have specific solubility characteristics which, with their shape and pH of the urine (and of course, clinical history), can aid in their identification. Sometimes, despite doing these solubility studies, the identity of the crystal remains a mystery. The clinical relevance of such crystals is questionable, but drug or chemical toxicity should always be considered in an animal presenting with clinical signs of renal failure and unidentified crystals in the urine.
- Melamine: The crystals shown in the image on the right were seen in the urine of a cat with acute renal failure due to melamine toxicosis. These crystals were highly characteristic of melamine and facilitated diagnosis in affected animals.
- Allantoin: Allantoin crystals were identified in a urine from a dog with acute myeloid leukemia (Meichner et al 2015). They were colorless to yellow-brown long rectangular thin needle-like crystals, clustered together in a fan- or “sheaf of wheat”-like arrangement.
- Xanthine: These can be seen in the urine of animals being treated with allopurinal, e.g. dalmations. They resemble ammonium biurate in that they are yellow to brown spheres, but they do appear to have concentric striations and lack the projections of ammonium biurate. They dissolve in sodium hydroxide (1 M) but not in acetic acid or hydrochloric acid (Uchiumi Davis and Grindem 2015) In contrast, ammonium biurate dissolve slowly in hydrochloric and acetic acid forming uric acid crystals and are fully soluble in NaOH, releasing ammonia. They also dissolve slowly on heating (Haber 1934). Xanthine calculi have been reported in Cavalier King Charles spaniels (van Zuilen et al 1997) and other breeds (University of Minnesota).
- Leucine and tyrosine: Leucine and tyrosine crystals have been reported in the urine of human patients with liver disease. To our knowledge (PubMed search), neither of these crystals have documented in animal patients with liver disease. We have certainly not identified or recognized them at Cornell University. Leucine are round to oval yellowish-brown crystals with circular striations on their edges (given them a somewhat crimped outline) whereas tyrosine are colorless thin needle-like crystals in bundles and can be mistaken for other needle-like crystals. Both occur in acid urine.
- Uric acid: Rarely seen in urine from animals, this crystal takes on various forms but is most commonly seen as irregular rectangles (called “whetstones”), which can be flat or laminated, and may form rosettes. Other forms include ovals with pointed ends (“lemon”-shaped), barrels, cubes, “hammers”, six-sided forms resembling cystine and sheaves of thin long rectangles, among other unusual shapes. They are strongly birefringent with polarized light, which helps differentiate them from cystine, which does not polarize. Uric acid forms in acidic urine and amorphous urates can be converted into uric acid with the addition of glacial acetic acid.
Solubility characteristics
Solubility features in strong acids and alkali can help differentiate between crystal types (Harber 1934).
| Crystal | Hydrochloric acid | Acetic acid | Sodium hydroxide | Heat |
| Struvite | Soluble | Soluble in dilute acid | Insoluble | Insoluble |
| Calcium oxalate | Soluble in dilute | Insoluble | Slight | Soluble |
| Ammonium biurate | Soluble (make uric acid) | Converts to uric acid | Soluble (releases ammonia) | Soluble |
| Calcium carbonate | Soluble (liberates carbon dioxide) | Soluble (liberates carbon dioxide as gas bubbles) | Insoluble | Insoluble |
| Uric acid | Insoluble | Insoluble | Soluble (10%) | Soluble at 60C |
| Calcium phosphate | Soluble in dilute HCl | Soluble | Insoluble | Insoluble (to 60C) |
| Cystine | Soluble | Insoluble | Soluble | – |
| Xanthine | Insoluble | Insoluble | Soluble (1 N) | – |
| Sulfa | – | Soluble in strong, insoluble in dilute | Soluble | – |
Related links
- Crystal quick guide: Compilation tables of common and uncommon urine crystals.
- Urinalysis atlas
- References:
- Haber MH. Urinary sediment: A textbook Atlas. Educational Products Division, American Society of Clinical Pathologists, Chicago, 1934 (oldie but goodie, with a great table on dissolution features of crystals).
- Haber MH et al. Color atlas of the urinary sediment. An illustrated field guide based on proficiency testing. College of American Pathologists, Associated Press, 2010.
- Osborne CA and Stevens JB: Urinalysis: A clinical guide to compassionate patient care.
- Ringsrud KM and Linné JJ. Urinalysis and body fluids. A color text and atlas. Mosby, 1995.
